HRV Explained: What It Is and How to Improve It
Your heart does not beat like a metronome. Even when you feel completely relaxed, the time between each heartbeat varies slightly, sometimes by just a few milliseconds. This subtle variation, known as heart rate variability or HRV, has emerged as one of the most valuable biomarkers for understanding your overall health, stress resilience, and recovery capacity.
Heart rate variability provides a window into how well your autonomic nervous system is functioning. It reveals whether your body is stuck in a state of chronic stress or whether it can flexibly adapt to the demands of daily life. Athletes use HRV to optimize training schedules and prevent overtraining.
Health professionals examine it as an indicator of cardiovascular health and mental well-being. Everyday people are now tracking it through wearable devices to make informed decisions about sleep, exercise, and stress management.
Understanding HRV matters because it connects directly to how you feel and perform each day. When your HRV is low, you might notice fatigue, brain fog, and difficulty recovering from workouts. When it is high, you often experience more energy, better focus, and greater emotional resilience. The good news is that HRV is not fixed. Through targeted lifestyle changes, you can actively improve your heart rate variability and, by extension, your overall wellness.
This comprehensive guide will explain exactly what HRV is, how it reflects the health of your nervous system, and what factors influence it most significantly. More importantly, you will learn practical, evidence-based strategies to improve your HRV starting today.
What Is Heart Rate Variability (HRV)?
Defining HRV
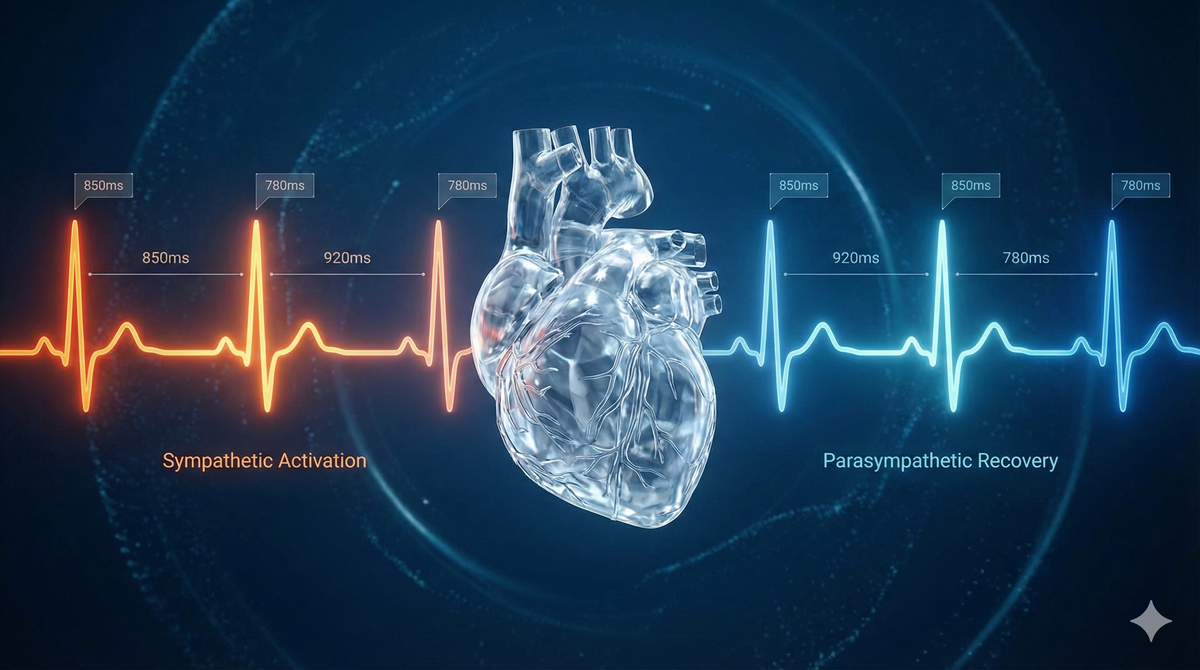
Heart rate variability refers to the variation in the time intervals between consecutive heartbeats. To understand this concept, imagine your heart beating 60 times per minute. You might assume that means one beat every second, but in reality, the intervals between beats constantly fluctuate. One interval might be 0.95 seconds, the next 1.05 seconds, then 0.98 seconds, and so on. These tiny variations, measured in milliseconds, constitute your HRV.
It is crucial to distinguish between heart rate and heart rate variability because they represent fundamentally different measurements. Heart rate tells you how many times your heart beats per minute. Heart rate variability tells you about the pattern and rhythm of those beats. Two people can have identical heart rates of 65 beats per minute, but vastly different HRV values.
A common misconception is that a steady, metronomic heartbeat indicates good health. The opposite is actually true. A heart that beats with rigid consistency often signals that the body is under stress or that the nervous system has lost some of its adaptive flexibility. Greater variability between beats typically reflects a healthier, more resilient cardiovascular system that can respond appropriately to changing demands.
The reason HRV matters so much is that it directly reflects the activity of your autonomic nervous system. When your body needs to respond to a threat or challenge, your sympathetic nervous system accelerates your heart rate and reduces variability. When you are safe, relaxed, and recovering, your parasympathetic nervous system slows your heart and increases variability. HRV essentially captures this ongoing dance between activation and recovery.
How HRV Is Measured
Heart rate variability measurement focuses on the precise timing between heartbeats, specifically the intervals between R waves on an electrocardiogram. These R-R intervals, also called interbeat intervals, are recorded in milliseconds and analyzed to produce various HRV metrics.
The gold standard for HRV measurement involves electrocardiogram (ECG) equipment used in clinical and research settings. These devices use electrodes placed on the chest to capture the electrical activity of the heart with extreme precision. However, technology has advanced to make HRV tracking accessible to anyone.
Chest strap heart rate monitors provide highly accurate HRV data because they detect the electrical signals of the heart directly. Many athletes and serious health trackers prefer this method for its reliability. Popular options include monitors from Polar and other fitness technology companies that pair with smartphone apps for analysis.
Smartwatches and fitness trackers have made HRV monitoring mainstream. Devices from companies like Apple, Garmin, Fitbit, and Whoop use optical sensors called photoplethysmography to detect blood flow changes in your wrist. While slightly less precise than chest straps or ECG devices, these wearables provide valuable HRV data that is more than adequate for tracking trends over time.
Dedicated HRV devices and apps offer another option. Some products specifically focus on HRV measurement and analysis, providing detailed insights and guided improvement protocols. These often use finger sensors or smartphone camera technology to capture pulse wave data.
When you see HRV data from these devices, you will encounter several common metrics:
- RMSSD (Root Mean Square of Successive Differences) represents the most commonly reported HRV metric for short-term recordings. It measures the variability between consecutive heartbeats and strongly reflects parasympathetic nervous system activity. Higher RMSSD values generally indicate better recovery and lower stress.
- SDNN (Standard Deviation of NN Intervals) captures overall heart rate variability and reflects both sympathetic and parasympathetic influences. This metric requires longer recording periods to be meaningful, typically 24 hours for clinical purposes.
- HRV Score is a simplified, proprietary number that many consumer devices provide. Companies like Whoop, Oura, and others process raw HRV data through algorithms to generate an easy-to-understand score, often on a scale of 1-100 or expressed in milliseconds.
For most people tracking HRV at home, consistency matters more than the specific metric used. Measuring at the same time each day, ideally upon waking or during sleep, produces the most reliable and comparable data.
What Your HRV Numbers Mean
Interpreting HRV can initially seem confusing because there is no single "normal" value that applies to everyone. Heart rate variability varies enormously based on age, fitness level, genetics, and individual physiology. A healthy 25-year-old athlete might have an HRV of 80 milliseconds or higher, while a healthy 55-year-old office worker might hover around 30 milliseconds. Both could represent optimal health for each individual.
Generally speaking, higher HRV values indicate greater parasympathetic activity and better adaptive capacity. A high HRV suggests that your body can effectively shift between states of activation and recovery. It typically correlates with good cardiovascular fitness, low chronic stress, adequate sleep, and overall resilience.
Lower HRV values suggest increased sympathetic dominance or reduced parasympathetic activity. When HRV drops below your personal baseline, it often signals that your body is dealing with stress, whether from physical exertion, poor sleep, illness, emotional strain, or other factors. Chronically low HRV has been associated with increased risk for cardiovascular disease, anxiety, depression, and reduced overall well-being.
The most important principle for interpreting HRV is to focus on your personal baseline rather than comparing yourself to others. Your optimal HRV is unique to you. What matters most is how your current readings compare to your own historical averages and trends.
Tracking HRV over weeks and months reveals meaningful patterns. You might notice that your HRV consistently drops after poor sleep, rises after restful weekends, or tanks during particularly stressful work periods. These personal insights become far more valuable than any population-level comparison.
Most wearable devices and apps help establish your baseline HRV by analyzing several days or weeks of data. Once your baseline is established, you can interpret daily variations in context. A reading 10-15% below your baseline might suggest that today is better suited for rest than intense training. A reading above baseline might indicate that your body is well-recovered and ready for challenge.
Why HRV Matters — The Nervous System Connection
HRV and the Autonomic Nervous System
To truly understand heart rate variability, you need to understand the autonomic nervous system (ANS). This branch of your nervous system operates largely below conscious awareness, controlling vital functions like heart rate, breathing, digestion, and blood pressure. The ANS has two main divisions that work in constant dynamic balance.
The sympathetic nervous system governs your fight or flight response. When activated, it prepares your body for action or threat. Your heart beats faster and more regularly, blood pressure rises, breathing quickens, digestion slows, and stress hormones flood your system. This response evolved to help humans survive immediate physical dangers, but modern life triggers it constantly through work deadlines, traffic, financial worries, and countless other non-physical stressors.
The parasympathetic nervous system controls your rest and digest functions. When dominant, it promotes recovery, relaxation, and restoration. Your heart rate slows, heart rate variability increases, digestion becomes active, and your body focuses on repair and regeneration. The vagus nerve, the primary pathway of the parasympathetic system, plays a crucial role in this process. The strength of vagus nerve activity is often referred to as vagal tone, and higher vagal tone correlates strongly with higher HRV.
Heart rate variability serves as a real-time readout of autonomic nervous system balance. When the parasympathetic system is active and you have strong vagal tone, your heart rate varies significantly between beats. When the sympathetic system dominates, your heart beats more uniformly with less variation. By measuring HRV, you are essentially measuring how much influence each branch of the ANS has over your heart at any given time.
Healthy autonomic function requires the ability to shift smoothly between these states depending on circumstances. You need sympathetic activation to exercise, meet deadlines, and handle emergencies. You need parasympathetic dominance to sleep deeply, digest food, recover from workouts, and maintain emotional equilibrium. Problems arise when one branch dominates inappropriately, particularly when chronic sympathetic activation prevents adequate recovery.
Modern life tends to push most people toward sympathetic dominance. Constant connectivity, work pressure, sleep deprivation, and sedentary lifestyles all contribute to keeping the nervous system in a state of low-grade chronic stress. This imbalance manifests as reduced HRV and increased vulnerability to physical and mental health problems.
HRV as a Window Into Recovery and Stress
One of the most valuable aspects of HRV tracking is its ability to reveal your recovery status and stress load. Your HRV reading essentially answers the question: Is my body in a state of stress or a state of recovery?
Recovery encompasses far more than just rest after exercise. It includes your body's ability to repair tissue, regulate inflammation, consolidate memories, balance hormones, and restore energy reserves. All of these processes occur most effectively when the parasympathetic nervous system is dominant and HRV is elevated.
When you see your HRV trending upward over time, it typically indicates that your body is adapting positively to the demands you are placing on it. Your nervous system has the flexibility to recover effectively and prepare for future challenges. This reflects overall resilience, the ability to handle stress without being overwhelmed by it.
When HRV trends downward or remains chronically suppressed, it suggests that recovery is compromised. Your body may be accumulating stress faster than it can recover from it. This happens when physical training exceeds recovery capacity, when sleep is insufficient, when psychological stress is unrelenting, or when illness is present.
Athletes have embraced HRV tracking precisely because it reveals this recovery-stress balance. A low HRV reading on a morning when you planned an intense workout might suggest backing off to prevent overtraining. A high HRV reading might indicate green light for pushing harder. This objective data removes guesswork from training decisions and helps prevent the injury and burnout that come from ignoring recovery needs.
Beyond athletic performance, HRV provides similar insights for everyday stress management. You might notice that your HRV drops significantly during high-pressure work periods, signaling that stress reduction strategies should become a priority. Or you might observe that vacations and weekends consistently elevate your HRV, confirming the importance of rest and leisure.
The connection between HRV and stress response also extends to acute situations. When you encounter a stressor, your HRV drops as the sympathetic system activates. After the stressor passes, your HRV should recover as the parasympathetic system regains control. The speed and completeness of this recovery reflect your nervous system regulation capacity. People with higher baseline HRV tend to recover from acute stress more quickly and completely.
HRV as a Health and Performance Indicator
Heart rate variability has emerged as a valuable biomarker because it correlates with such a wide range of health outcomes. Researchers and clinicians increasingly recognize HRV as a window into overall physiological well-being.
HRV can indicate the following:
- Stress levels: Lower HRV consistently correlates with higher perceived stress and elevated stress hormone levels. Tracking HRV can help you identify stress before it becomes overwhelming.
- Recovery status: Your current HRV compared to your baseline reveals how well-recovered you are from recent physical and mental demands. This informs decisions about training intensity, work capacity, and need for rest.
- Fitness adaptation: Over weeks and months, rising HRV often indicates that your cardiovascular system is becoming more efficient and your fitness is improving. Regular aerobic exercise typically produces measurable increases in resting HRV.
- Sleep quality: Because HRV is strongly influenced by sleep, your readings can confirm whether your sleep is actually restorative. Poor HRV despite adequate sleep hours might indicate issues with sleep quality that warrant investigation.
- Cardiovascular health: Research has linked chronically low HRV to increased risk of cardiovascular disease, hypertension, and cardiac events. While HRV alone cannot diagnose heart problems, sustained low values may warrant medical evaluation.
- Mental health status: Lower HRV has been associated with anxiety disorders, depression, and reduced emotional regulation capacity. Improving HRV through lifestyle interventions often corresponds with improved mental health symptoms.
- Illness and inflammation: Your HRV often drops when your immune system is fighting infection or dealing with inflammation. Some people notice their HRV decline before they consciously feel sick, providing early warning of impending illness.
- Aging trajectory: HRV typically decreases with age, but the rate of decline varies significantly between individuals. Maintaining higher HRV into older age correlates with better health outcomes and potentially slower biological aging.
- Training readiness: For athletes and fitness enthusiasts, morning HRV indicates whether the body is prepared for intense training or would benefit from lighter activity or rest.
The accumulation of this evidence has positioned HRV as one of the most comprehensive single metrics available for monitoring overall health and performance. While it should not replace medical care or be used as a diagnostic tool without professional guidance, HRV tracking empowers individuals to make better daily decisions about exercise, stress management, and recovery priorities.
Key Factors That Impact HRV
Sleep Quality and Duration
Sleep stands as perhaps the single most important factor influencing heart rate variability. The connection between sleep and HRV runs deep because sleep is when your parasympathetic nervous system should dominate and when most recovery and restoration occur.
During sleep, particularly during deep sleep and REM sleep stages, your body activates parasympathetic pathways and suppresses sympathetic activity. This shift allows HRV to rise, reflecting the recovery work happening throughout your body. Proteins are synthesized, memories are consolidated, hormones are balanced, and cellular repair accelerates.
When sleep is insufficient or poor quality, this recovery process is disrupted. Your HRV suffers as a direct result. Research consistently shows that sleep deprivation causes measurable drops in HRV, sometimes dramatic ones. Even a single night of poor sleep can lower your HRV the following day, and chronic sleep restriction produces sustained HRV suppression.
Sleep quality matters as much as sleep duration. You can spend eight hours in bed but if you are waking frequently, not reaching deep sleep stages, or experiencing sleep apnea, your HRV will not benefit as it should. The amount of time spent in deep sleep and REM sleep strongly predicts overnight HRV improvements.
Factors that disrupt sleep quality and harm HRV include:
- Irregular sleep schedules that disrupt circadian rhythm
- Alcohol consumption, especially close to bedtime
- Late-night eating that diverts energy to digestion
- Screen exposure and blue light in the hours before sleep
- Caffeine consumed too late in the day
- Sleeping in environments that are too warm, noisy, or bright
- Unmanaged stress and anxiety that prevents mental unwinding
- Sleep disorders like sleep apnea, insomnia, or restless leg syndrome
The relationship between sleep and HRV is bidirectional. Poor sleep lowers HRV, but low HRV can also indicate disrupted sleep architecture. Many wearable devices now track both sleep stages and HRV together, allowing you to see these connections clearly in your own data.
Stress and Mental Health
Chronic stress represents one of the most common and damaging suppressors of heart rate variability. When stress becomes persistent rather than occasional, the sympathetic nervous system remains activated far longer than it should, crowding out the parasympathetic activity needed for recovery.
The stress response evolved to help humans survive acute physical threats. When activated briefly and then resolved, it causes no lasting harm. Problems emerge when modern psychological stressors keep the system engaged continuously. Work pressure, financial concerns, relationship difficulties, social media comparison, and information overload all trigger stress responses that rarely fully resolve.
This chronic sympathetic activation directly suppresses HRV. Studies consistently find that people reporting high stress levels have lower HRV than their less-stressed counterparts. Moreover, interventions that reduce perceived stress typically produce corresponding increases in HRV.
The relationship between HRV and mental health conditions deserves particular attention. Anxiety disorders are strongly associated with reduced HRV, reflecting the constant sympathetic hyperactivation that characterizes anxiety. Depression also correlates with lower HRV, possibly due to autonomic dysregulation that accompanies the condition. Importantly, successful treatment of these conditions often corresponds with HRV improvements.
Emotional state affects HRV on a moment-to-moment basis as well. Anger, frustration, and fear reduce HRV almost immediately. Positive emotions like gratitude, compassion, and contentment tend to support higher HRV. This emotional-physiological connection explains why mood management and emotional regulation matter for nervous system health.
Trauma history can leave lasting imprints on HRV patterns. People with post-traumatic stress disorder typically show reduced HRV, reflecting a nervous system stuck in protective mode. Trauma-informed therapies often aim to restore healthy autonomic function as part of healing.
The good news is that stress management interventions reliably improve HRV. Practices like meditation, mindfulness, time in nature, social connection, and cognitive behavioral strategies have all demonstrated ability to shift the autonomic balance toward parasympathetic dominance. You cannot always control the stressors in your life, but you can develop tools to regulate your response to them.
Hydration and Nutrition
The role of hydration in heart rate variability often goes underappreciated. Proper hydration directly affects blood volume, blood viscosity, and cardiovascular function, all of which influence HRV readings and actual autonomic function.
When you are dehydrated, blood volume decreases. Your heart must work harder to circulate the thicker, reduced blood supply, requiring increased sympathetic activation. This shows up as elevated heart rate and suppressed HRV. Even mild dehydration that you might not consciously notice can produce measurable effects on your heart rate variability.
Electrolyte balance matters alongside fluid intake. Sodium, potassium, magnesium, and other electrolytes regulate fluid distribution and nerve function. Electrolyte imbalances can disrupt the electrical signals that control heart rhythm and variability. This is why hydration advice increasingly emphasizes electrolyte-containing fluids rather than water alone, especially for active individuals or those in hot climates.
The impact of dehydration on HRV can confound your data interpretation. A low HRV reading might reflect genuine stress or poor recovery, or it might simply indicate that you did not drink enough water yesterday. Maintaining consistent hydration helps ensure your HRV readings accurately reflect your nervous system state rather than fluid status.
Nutrition affects HRV through multiple pathways. Certain substances have acute negative effects on heart rate variability:
- Alcohol deserves special mention because its impact on HRV is substantial and well-documented. Even moderate alcohol consumption suppresses HRV, particularly overnight HRV. Alcohol interferes with sleep architecture, preventing the deep sleep stages where parasympathetic activity should dominate. Regular drinkers often see their HRV rise significantly when they reduce or eliminate alcohol.
- Caffeine in excessive amounts or consumed too late in the day can stimulate the sympathetic nervous system and reduce HRV. Individual sensitivity varies widely, so tracking your own HRV response to caffeine can reveal your personal tolerance.
- Highly processed foods and diets high in sugar and refined carbohydrates have been associated with lower HRV in research studies. The mechanisms likely involve inflammation, blood sugar instability, and metabolic stress.
- Large meals, especially eaten late in the evening, direct blood flow to the digestive system and can suppress overnight HRV. The timing and size of meals influences how effectively your body can shift into recovery mode during sleep.
Conversely, certain nutritional factors support healthy HRV. Anti-inflammatory foods rich in omega-3 fatty acids, antioxidants, and fiber appear to support autonomic function and HRV. The Mediterranean diet pattern has shown favorable associations with HRV in research. Adequate micronutrient intake, particularly magnesium, supports healthy nervous system function and HRV.
Physical Activity and Exercise
The relationship between physical activity and heart rate variability is complex but ultimately favorable. Regular exercise is one of the most effective ways to improve HRV over time, but the timing and intensity of exercise matter significantly.
Aerobic exercise, performed consistently over weeks and months, produces reliable increases in resting HRV. Running, cycling, swimming, and other cardiovascular activities challenge the heart and nervous system, prompting adaptations that enhance vagal tone and parasympathetic capacity. These adaptations represent improved cardiovascular fitness and recovery ability.
The mechanism involves improved autonomic modulation. Fit individuals develop stronger parasympathetic reactivation after stress, meaning their nervous systems can shift out of sympathetic dominance more quickly and completely. This shows up as higher resting HRV and faster HRV recovery after exercise.
Sedentary lifestyles produce the opposite effect. Chronic inactivity is associated with persistently low HRV and reduced cardiovascular health. Even independent of other factors, simply spending too much time sitting and too little time moving impairs autonomic function.
However, acute intense exercise temporarily decreases HRV. During and immediately after hard workouts, your sympathetic nervous system is highly activated, and HRV drops accordingly. This is normal and expected. The concern arises when recovery from exercise is inadequate.
Overtraining represents a state where training stress exceeds recovery capacity over an extended period. One of the hallmark signs of overtraining is chronically suppressed HRV that does not rebound between workouts. Athletes who ignore this signal risk injury, illness, performance decline, and burnout.
The key principle is that exercise benefits HRV when balanced with adequate recovery. High training loads require proportionally more attention to sleep, nutrition, stress management, and rest days. The goal is to challenge your body enough to stimulate adaptation without exceeding your recovery capacity.
Breathing Patterns
The connection between breathing and heart rate variability is direct and powerful. Your respiratory pattern immediately influences your autonomic nervous system balance and HRV readings.
Every breath you take modulates your heart rate in a phenomenon called respiratory sinus arrhythmia. When you inhale, your heart rate naturally increases slightly as sympathetic activity rises. When you exhale, your heart rate decreases as parasympathetic activity strengthens. This rhythmic variation contributes significantly to overall HRV.
Slow, deep breathing maximizes this effect and shifts autonomic balance toward parasympathetic dominance. When you deliberately slow your breathing to around six breaths per minute, you create optimal conditions for heart rate variability. This breathing rate appears to produce resonance between respiratory and cardiovascular rhythms, amplifying parasympathetic activation.
In contrast, rapid, shallow breathing, which characterizes stressed states, activates the sympathetic system and suppresses HRV. Many people chronically breathe too quickly and too shallowly without realizing it, maintaining subtle sympathetic activation throughout the day.
The vagus nerve, the primary parasympathetic pathway, is directly influenced by breathing mechanics. Long, slow exhalations stimulate vagus nerve activity and increase vagal tone. This explains why breathing exercises are among the fastest-acting interventions for improving HRV.
How to Improve Your HRV
Prioritize Quality Sleep
Improving your sleep is the foundation of any HRV improvement strategy. Given the profound impact of sleep on parasympathetic recovery, no amount of other interventions can compensate for chronically poor sleep. Follow these step-by-step actions to optimize your sleep for HRV improvement:
- Set a consistent sleep schedule. Choose a target bedtime and wake time and maintain them within thirty minutes every day, including weekends. Consistency reinforces your circadian rhythm and improves sleep quality.
- Create an optimal sleep environment. Make your bedroom as dark as possible using blackout curtains or an eye mask. Keep the temperature cool, ideally between 65 and 68 degrees Fahrenheit. Minimize noise with earplugs or a white noise machine if necessary.
- Establish a wind-down routine. Begin relaxing activities sixty to ninety minutes before bed. Dim lights throughout your home to signal your brain that sleep is approaching. Avoid stimulating content like intense movies, work emails, or social media.
- Limit screen exposure before bed. The blue light from phones, tablets, and computers suppresses melatonin production. Stop using screens at least one hour before bed, or use blue light blocking glasses and device settings if screen use is unavoidable.
- Watch what and when you eat. Finish eating at least two to three hours before bed. Avoid heavy meals in the evening. Limit fluids close to bedtime to prevent sleep disruptions from bathroom visits.
- Eliminate or drastically reduce alcohol. Even moderate drinking severely impairs sleep quality and overnight HRV. If you choose to drink, do so earlier in the day and in small amounts, recognizing the trade-off.
- Manage caffeine intake. Stop consuming caffeine by early afternoon at the latest. Individual sensitivity varies, so track how caffeine affects your sleep and adjust accordingly.
- Get morning light exposure. Bright light in the first hour after waking helps regulate your circadian rhythm, which improves sleep quality that night. Spend time outdoors or use a light therapy device.
- Exercise regularly but not too late. Physical activity improves sleep quality, but intense exercise close to bedtime can interfere with sleep onset. Aim to finish vigorous workouts at least three to four hours before bed.
- Address sleep disorders. If you snore, gasp during sleep, feel unrefreshed despite adequate sleep hours, or have persistent insomnia, consult a healthcare provider. Conditions like sleep apnea dramatically impair HRV and overall health.
Manage Stress Effectively
Because chronic stress is such a potent suppressor of HRV, developing effective stress management strategies is essential for improving your readings and overall nervous system health. Proven stress-reduction techniques include:
- Meditation: Regular meditation practice increases parasympathetic activity and improves HRV over time. Even brief daily sessions produce benefits. Guided meditation apps make starting easy for beginners.
- Mindfulness: Bringing non-judgmental awareness to present moment experience helps interrupt stress cycles. Practicing mindfulness throughout daily activities gradually builds nervous system resilience.
- Time in nature: Spending time in natural environments reduces stress hormones and supports parasympathetic activation. Even brief exposure to green spaces or natural sounds produces measurable benefits.
- Social connection: Positive social interactions activate the parasympathetic system and reduce stress. Prioritize meaningful time with supportive friends and family.
- Journaling: Writing about thoughts, feelings, and stressors provides emotional processing that reduces the physiological burden of stress. Gratitude journaling specifically has shown benefits for well-being and potentially HRV.
- Cognitive reframing: Learning to interpret challenging situations in less threatening ways reduces the intensity of stress responses. Cognitive behavioral techniques teach this skill systematically.
- Limiting news and social media: Constant exposure to negative information maintains stress activation. Setting boundaries around consumption protects your nervous system.
- Hobbies and play: Engaging in enjoyable activities for their own sake promotes positive emotions and parasympathetic states. Make time for activities that bring you joy.
Stay Properly Hydrated
Maintaining proper hydration supports accurate HRV readings and genuine autonomic function. Follow these simple guidelines:
- Drink consistently throughout the day rather than consuming large amounts at once. Steady hydration maintains blood volume more effectively.
- Use thirst as a starting point but recognize that it is not always a reliable indicator, especially during exercise or in hot conditions. Proactive drinking is often necessary.
- Include electrolytes in your hydration strategy, particularly if you exercise, sweat heavily, or eat a low-sodium diet. Sodium, potassium, and magnesium all support fluid balance and nerve function.
- Monitor urine color as a simple hydration indicator. Pale yellow suggests adequate hydration while darker colors indicate a need for more fluids.
- Start each day with water. Drinking upon waking helps replenish fluids lost overnight and supports morning HRV readings.
Practice Breathing Exercises
Breathwork offers one of the fastest and most accessible methods for improving heart rate variability. The following techniques have demonstrated ability to activate the parasympathetic nervous system and increase HRV.
Box Breathing:
Box breathing, also called square breathing, uses equal duration for each phase of the breath. This technique is used by military personnel, athletes, and performers to manage stress and enhance focus. Step-by-step instructions:
- Sit or lie in a comfortable position with a straight spine.
- Exhale completely through your mouth, emptying your lungs.
- Inhale slowly through your nose for a count of four seconds.
- Hold your breath with lungs full for a count of four seconds.
- Exhale slowly through your mouth for a count of four seconds.
- Hold your breath with lungs empty for a count of four seconds.
- Repeat this cycle for four to eight minutes.
Slow Diaphragmatic Breathing:
This technique emphasizes deep belly breathing with extended exhalations to maximize parasympathetic activation. Step-by-step instructions:
- Place one hand on your chest and one on your belly.
- Breathe slowly through your nose, directing the breath into your belly. Your belly hand should rise while your chest hand stays relatively still.
- Inhale for four seconds, allowing your diaphragm to fully descend.
- Exhale slowly through pursed lips or your nose for six to eight seconds.
- The extended exhalation is key, as it stimulates the vagus nerve and activates the parasympathetic system.
- Continue for five to ten minutes.
Exercise Consistently but Wisely
Physical activity improves HRV over time when approached with appropriate balance between training stress and recovery. Guidelines for exercise that supports HRV:
- Establish a regular exercise habit. Consistency over weeks and months produces the aerobic adaptations that elevate resting HRV. Aim for at least 150 minutes of moderate aerobic activity weekly as a foundation.
- Progress gradually. Sudden large increases in training volume or intensity can overwhelm recovery capacity and suppress HRV. Follow the ten percent rule, increasing weekly training load by no more than ten percent.
- Include rest days. Your body adapts and improves during recovery, not during the workouts themselves. Schedule at least one to two complete rest days per week.
- Vary intensity. Not every workout should be hard. Include easy, recovery-paced sessions that build aerobic base without depleting recovery reserves.
- Listen to your body and HRV data. If your morning HRV is significantly below baseline and you feel fatigued, consider reducing planned workout intensity or taking an extra rest day.
Monitor and Track Your HRV
Consistent HRV tracking provides the objective feedback needed to understand what works for your body and to make informed lifestyle decisions. To establish your personal baseline, begin tracking HRV daily under consistent conditions. Collect at least one to two weeks of data before drawing conclusions. Popular HRV tracking tools and apps include:
- Whoop: A subscription-based wearable that provides detailed HRV, sleep, and recovery metrics with a focus on training readiness.
- Oura Ring: A ring-based tracker that measures HRV during sleep and provides daily readiness scores.
- Apple Watch: Offers HRV tracking through the Health app, with third-party apps providing additional analysis.
- Garmin devices: Many Garmin watches track HRV and provide Body Battery and other recovery metrics.
Focus on trends over time rather than obsessing over daily values. Use low HRV readings as information, not judgment. A low reading simply suggests your body is dealing with stress or needs recovery. Respond with self-compassion and appropriate adjustments.
Conclusion
Heart rate variability stands as one of the most valuable biomarkers available for understanding your body's state of stress and recovery. This simple measurement, the variation in time between heartbeats, reveals the complex dance between your sympathetic and parasympathetic nervous systems. It tells you whether your body is stuck in fight or flight mode or whether it can flexibly shift into rest and digest states that allow healing, adaptation, and resilience.
High HRV reflects a nervous system that can respond appropriately to challenges and recover effectively afterward. It correlates with cardiovascular health, stress resilience, emotional regulation, and overall well-being. Low HRV signals that something in your lifestyle or environment is preventing adequate recovery, whether that is poor sleep, chronic stress, dehydration, or overtraining.
The empowering truth about HRV is that it responds to lifestyle changes. Unlike genetic factors that you cannot modify, your heart rate variability improves when you sleep better, manage stress more effectively, stay properly hydrated, exercise appropriately, and practice breathing techniques that activate your parasympathetic system. Small, consistent changes accumulate into meaningful improvements over weeks and months.
You do not need to implement every strategy discussed in this article at once. Choose one or two areas where you see the greatest opportunity for improvement. As you make changes, track your HRV to see how your body responds. This feedback loop transforms abstract health advice into personalized, evidence-based optimization. You will learn what genuinely works for your unique physiology and what matters less.
Start today by choosing a measurement method that fits your lifestyle. Establish your baseline over the next one to two weeks. Then select one improvement strategy from this article and implement it consistently for several weeks while monitoring the results. Your nervous system is remarkably adaptable. With attention and appropriate inputs, it can shift from chronic stress dominance toward greater balance, flexibility, and resilience. Heart rate variability provides the window to observe this transformation happening, one heartbeat at a time.